How to use a super bill for potential insurance reimbursement for out-of-network healthcare
How do I use my insurance with inhaleMD?
At this time, due to the evolving legal status of cannabis, we cannot accept any insurance. This means that you pay us directly for your appointments. This means we are an “out of network provider” according to your insurance. We are not contracted with your insurance and reimbursement is not guaranteed unless specifically outlined in your policy. We can, however, provide you with a super bill that you can submit to your insurance for possible partial reimbursement.
What is a super bill?
A super bill is a document, like an invoice or receipt, that outlines the care that you received. It is not the same as the credit card receipt you will also receive (which will say Digital Bear Entertainment – don’t be confused). Do not submit the credit card receipt to your insurer. The super bill is generated by our electronic health system and sent to you by email following each visit wherein we take a payment. It must include the following information in order to be considered for reimbursement:
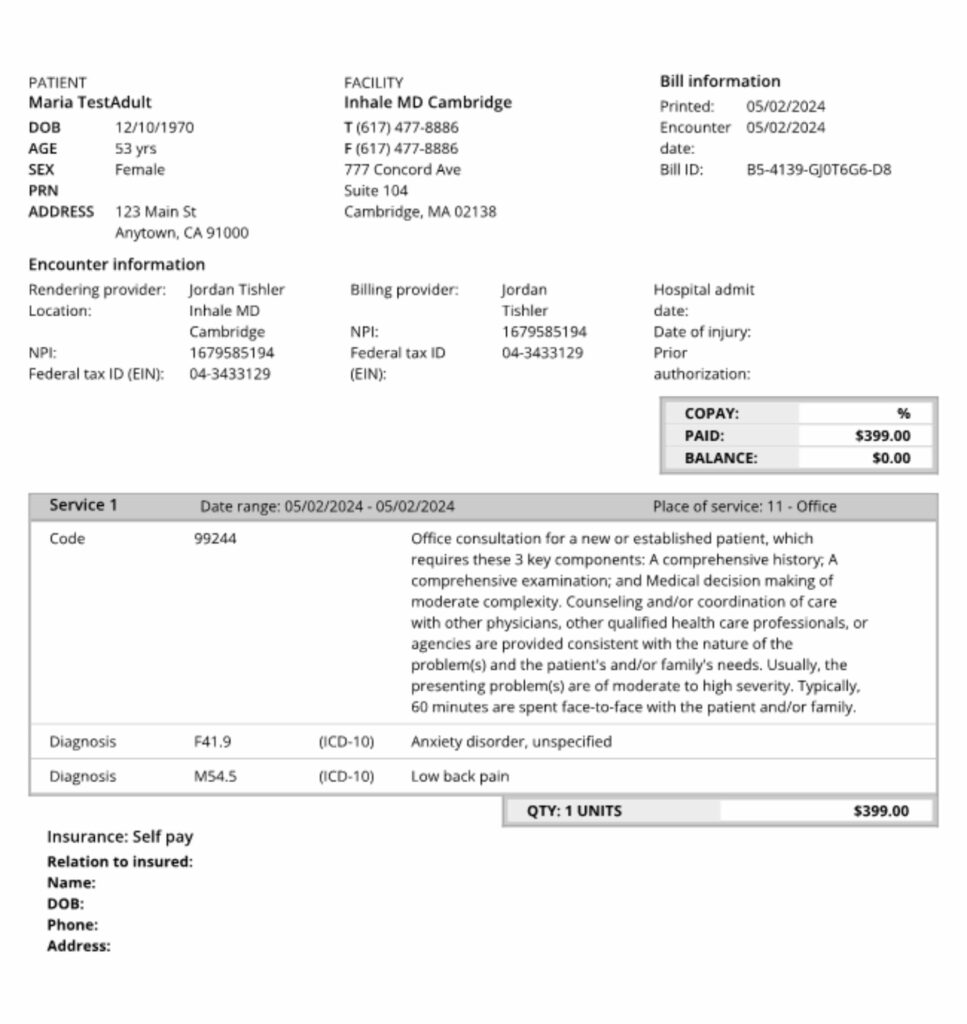
1. Client name, address, and date of birth
2. Physician name, phone number, and email
3. Physician Tax ID and National Provider Identifier (NPI)
4. Statement number and date issued to client
5. A diagnosis and diagnosis code (also called a CPT code)
6. Service type, date, and code for reimbursement
7. The fees that you paid
This is an example super bill:
What are some points to consider before I decide to submit a super bill to my insurance?
Reimbursement requires a diagnosis. The super bill will not mention cannabis or any form of treatment.
How do I submit my super bill?
When submitting your super bill, you must specify it as “an out of network office visit with a specialist”. Use these words exactly. If you don’t, it will likely be rejected.
Insurances typically have a time limit in which you can submit the super bill. This is usually 90-180 days – you should check with your insurance to be sure you don’t send it too late.
To submit your super bill, contact your insurance company and ask for “member services” or check their website for instructions. There are usually 3 options for turning in a super bill: mail, fax, or through an online portal.
-
-
- Mail – you can ask your insurance for an address to mail the super bill. Make sure you allow time for delivery to stay within your limit for timely filing.
- Fax – if you would like to keep your protected health information private, we suggest not faxing from a public fax machine (such as at the library) or a work fax machine. The receipt that shows your fax was sent will include this private health information.
- Online portal – most insurance providers will have an online portal through which you can upload your super bill. It is the most secure option to send your super bill as the website will request a login or password. It is also faster than mail or fax. Be sure to ask your insurance about this option.
-
What can you expect after you submit a super bill?
It can typically take your health insurance 2-4 weeks to process your super bill. If they accept your claim, they will either pay some amount for the services minus your copay, or they will put this amount towards your deductible if you have one.
Very commonly insurance companies will deny payment for out-of-network visits. If your super bill is denied, call your insurance and request information about the denial. You have the right to up to 3 appeals of this denial. It is critical that you appeal in order to have the super bill reviewed more thoroughly. Typically this would be a physician but may be an nurse practitioner. With each successive appeal the reviewer is likely to be a physician and more likely to approve the payment.
The insurance company is counting on the wasted time and aggravation of these appeals in hopes that you will simply accept no payment. Please take the time to appeal any denial so that you can be rightfully reimbursed.
